By Dr. Venkatraman Chandra-Mouli, Scientist, Adolescent Sexual and Reproductive Health, World Health Organization’s Department of Reproductive Health and Research and the Human Reproduction Programme.
“If my parents learn that I am pregnant, they will throw me out of the house.”
“I don’t need a lecture from you. Can you just give me some condoms?”
“My mother-in-law does not want me to take the pills and my husband does not want to oppose her.”
“I want to know what my son says to you. I am paying for this consultation. I will not wait outside.”
“I cannot tell my girlfriend about this infection. That is out of question.”
Training alone cannot prepare health workers to deal with questions like the ones above and other challenging situations they often face in providing sexual and reproductive health services to adolescents.
There is widespread acknowledgement that a competent and caring health worker is critical to the provision of adolescent-responsive health services. To achieve this, there is strong consensus that we need to invest in building and supporting the abilities of health workers to respond to their adolescent patients—and, where relevant, their caretakers—effectively and with sensitivity and respect.
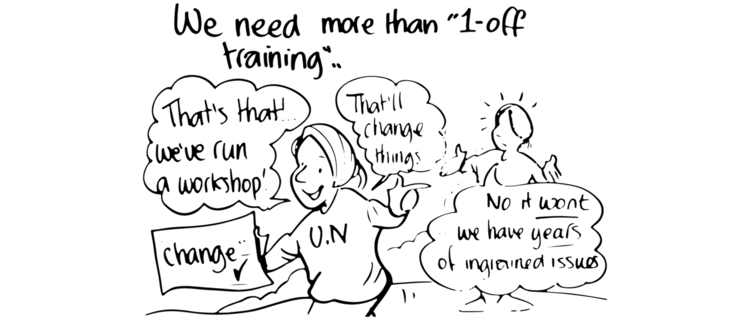
Almost universally, building competencies and empathy in health workers has been equated to training them. Calls for the training of health workers in various topics abound in global and regional agendas for action, in guidance from international organizations (including the World Health Organization), and in academic publications. The overwhelming emphasis on training is reflected in the volume of funding provided by donors, in investment cases,and in national policies and strategies.
Over the last 25 years enormous amounts of time, effort, and money have been invested to train health workers to be more “adolescent-friendly.” The results—from the perspectives of their clients and patients—are overwhelmingly disappointing.
A recent review we published reiterates the widespread consensus that inadequate knowledge and skills hinders the ability of health workers to provide adolescents with appropriate health services effectively, and that judgmental and disrespectful behaviors of health workers are a major barrier to adolescents seeking care initially or returning for follow-up services.
We need to take a step back and question our approach to training. This is critical for two reasons.
Firstly, training health workers alone does not lead to tangible improvements in health worker performance. There is convincing evidence that without ongoing, complementary support, learning that occurs in workshop settings will not translate into changes of practice in the work place. Despite such evidence, training alone persists as the current model and is often the only capacity building approach used.
Secondly, training programs which have focused curricula, involve small groups, and are conducted by skilled trainers using multiple methods have been shown to be more effective in promoting positive attitudes and in improving health workers’ knowledge, understanding, and skills. However, the pressure to train large numbers of health workers in short time periods generally means that important interactive and participatory elements—crucial to practicing application of knowledge and building skills—are omitted because of logistical, time, and financial constraints. Further, trainings within cascade training models rapidly deteriorate in quality because both the trainers and the training venue and/or equipment are often inadequate.
In addition, there is the added potential for inaccurately transmitted messages as there is little, if any, supervision and mentoring support.
What do we need to do differently, then?
We should put an end to off-site, one-off in-service training programs. We should replace these training initiatives with a combination of pre-service training and ongoing, off- and on-site training (with a preference for the latter).
We should ensure that training initiatives have limited and clearly defined objectives, involve small groups, and use multiple methods, with an emphasis on participatory and interactive elements. Training should be carefully monitored to ensure they are carried out with quality and fidelity.
We should combine high-quality trainings with other proven approaches including job descriptions grounded in quality standards, pocket and desk reference tools, supportive supervision, and peer-sharing and collaborative learning. Job descriptions and standards can provide clarity to health workers on expectations and accountability in their scope of work. Handy, clear, and credible pocket and desk reference tools can also serve as a friendly reminder to health workers what they need to do in practice. Supervision that is consistent, specific, and supportive—building competence and confidence on the one hand, and ensuing accountability on the other—can have a significant positive impact on performance and satisfaction. Finally, ongoing peer-sharing and collaborative learning in a safe environment can address deep-seated biases that are difficult to address let alone overcome, stimulate bottom-up problem definition and problem solving, and foster the development of norms and practices that are respectful and equitable in a group setting (even when they are not in the wider community in the group operates).
However, a word of caution. We must not replace one discredited magic bullet with another that is bound to fail. There are, in fact, no magic bullets. Even if health workers have the necessary competencies and positive attitudes, poor infrastructure, missing and/or broken equipment, and stock outs of medicines and other supplies will impede their ability to perform as desired. Furthermore, regardless of the quality of capacity building and support strategies used, overwhelming workloads, inadequate and untimely salary payments, and managerial arrogance and unfairness can rapidly lead to frustration and demotivation.
Providing good quality care to an infant with pneumonia and dealing with his/her parents with consideration calls for both technical abilities and interpersonal skills and qualities. However, responding to an adolescent who has initiated consensual sexual activity before the age of sexual consent, or one who is pregnant and does not want her parents to know, is more nuanced and complex. It requires the same abilities and qualities, as well as an awareness of laws and policies—and the broader social context—additional empathy and compassion, and appropriate handling of personal opinions and biases. We demand a lot from our health workers; in order for them to deliver, we need to do much more than we are to prepare and support them.